Physician Credentialing Services
Get your credentialing application accepted the first time…

Physician and Provider Credentialing Services
Physician credentialing and provider enrollment services is a process of enrolment and attestation that a physician is part of a Payer’s network and authorized to provide services to patients who are members in the Payer’s plans. Credentialing verifies that a physician meets standards as determined by the Payer by reviewing such items as the individual’s license, experience, certification, education, training, affiliations, malpractice & adverse clinical occurrences and clinical judgment.
Why opt for physician/provider credentialing services
Effective provider credentialing services are the absolute necessity for better performance of the practice. Without proper enrolment, payments can be delayed or refused by the insurance carriers, even if the physician is able to provide services that are competent and medically necessary.
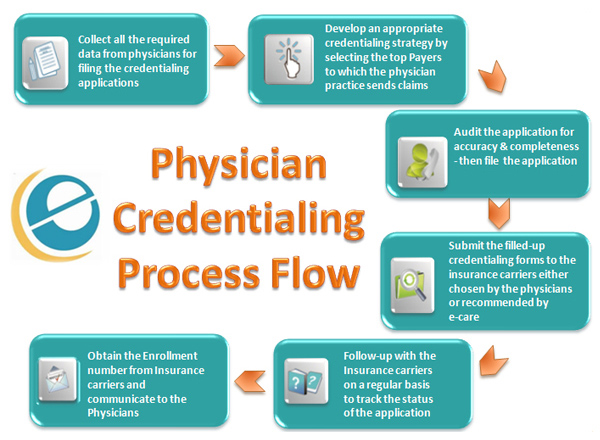
Click on the Image to zoom
We at e-care India offer Physician credentialing services, helping Providers achieve better revenues. Our tailor-made provider credentialing services facilitate the payer enrollment process when a Physicians
- Begin the first practice after Med school
- Change from one Practice to another
- Adding New Physician to an existing Group
- Want to become enrolled with a new Payer
Different Payers have their own set of forms to be filled either online or through paper applications. Once submitted, there should also be diligent follow-up with the Payers to ensure that the provider credentialing process is completed in the shortest time so that the revenues are not impacted.

The following process is followed as part of e-care’s physician credentialing services:
- Handling Provider letter of interest and application requisition from Payers
- New provider affiliations and Group Credentialing
- Facility Credentialing including addition of Providers to the Facility’s ID
- Preparation of paper CMS 855 and other Managed Care applications for all Payers including DME and Dental payers
- Preparation and submission of online applications to federal, state and commercial carriers
- Maintain and update specific Provider information directly with carriers at frequent intervals or when requested
- Resolve enrolment issues and track Managed Care contracts
- Preparation of contracting documents for scanning and Long-term storage electronically.
- Prepare, maintain and monitor Managed Care Summaries that Provides Effective dates, Fee Schedule details and Group affiliation.
- Monitoring Expiry dates for NYS-Registrations, DEAs, and CLIA registrations and also handling re-applications
- Handling Re-Credentialing whenever required
We ensure that your credentialing application gets the attention it deserves with our dedicated team of physician credentialing specialists

How much physician credentialing and provider enrollment services cost?
- In general & on average, expect to pay $2,000 - $5,000/year for physician credentialing services.
- Average cost is $150-300/physician, though this varies across credentialing service providers.
- Initial setup can cost between $200-800
- Per panel, expect to pay around $100 for an application
Do you want to know how much e-care charge?
Call us or Submit RFP to Get an Estimate for Physician Credentialing and provider enrollment services
Related Links
About Outsourcing
Our Expertise
More Info
Quick Facts
Affiliations
A Proud Member of HBMA