Prior Authorization

What is Prior Authorization Process?
Insurance Companies require the providers to obtain approval or permission before rendering certain medical services. This is to ensure the medical necessity of the treatment rendered. Not all services require Prior Authorization, a list of services that require prior authorization will be issued by each insurance.
The Utilization and Management Review department in the Insurance Company would issue the Prior Authorization after going through the treatment plan submitted by the provider. Emergency case is exceptional. Prior Authorization is otherwise called pre-certification.
Importance of Authorization
The Insurance Verification team plays a vital role and forms the base for the pre-authorization process. The Prior Authorization process optimizes revenue and helps with appropriate payment collection for services in the healthcare organization. Authorization does not guarantee any payment, but if the claim is denied we can submit an appeal with the authorization number for possible reimbursement from the insurance company. Lack of authorization can lead to financial liabilities for both the patient and the healthcare provider. Therefore having a partner like e-care to handle your medical billing and authorization process is the key towards increased reimbursement.
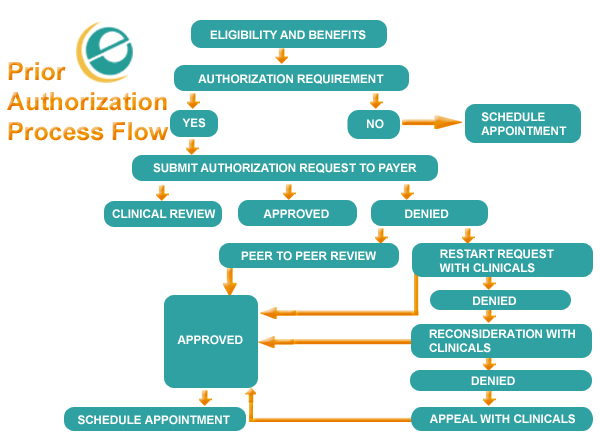
Click on the Image to zoom
Authorization Request process in e-care:
The best way to request authorization is through a phone call, VIA web portal, or by fax, depending on the insurance company's plan guidelines, and double-check that you meet all requirements before the requests are submitted online or by fax. e-care has a team of experienced Prior authorization team who understand the payor based nuances to get the best out of them and ensure the claims are process timely with maximum reimbursement. We also follow a standard checklist of information and documentations required depending upon the payor and insurance policy, to avoid last minute hassle. Listed below are basic information that is standard across most insurance companies to submit an authorization:
- Demographic information like the patient’s name, date of birth, address, and insurance ID number.
- Requesting and rendering provider information like NPI number, Tax ID number, phone number, fax number, and address.
- Servicing facility information where the services going to be performed whether in an office, Inpatient, or outpatient facility.
- CPT, HCPCS, and ICD 10 codes with descriptions.
- Length of stay for Inpatient requests.
- The insurance company may ask for some additional information on previous history of illness and the type of service provided.
- It’s mandatory to have the chief complaint for the patient also insurance may ask for the Clinical records for further clarification.
Authorization Requirement:
Prior Authorization requirements may vary based on the insurance plan-specific guidelines & place of service. In most cases, risky and expensive treatments require pre-approval from the insurance company, as those treatments involve cost efficiency & any mishandling will result in financial loss.
- A PCP referral is needed for HMO plans before submitting an authorization request to the insurance & the absence of a referral may result in the denial of an authorization request.
- The most of the insurance requires authorization for imaging services like MRI, MRA, CT, CTA, PET scan, etc.
- Few insurance companies have health consultants like Evicore, NIA, AIM specialty, American Health Group, etc. to handle authorization requests on their behalf.
- Outpatient emergency services do not require pre-authorization.
e-care follows a streamlined process for efficient process and result in prior authorization which indirectly helps faster claim processing and increased cash flow.

Related Links
About Outsourcing
Our Expertise
More Info
Quick Facts
Affiliation
A Proud Member of HBMA